About The Restorative Leadership Symposium
The Restorative Leadership Symposium, hosted by the Ministry of Health, Health Quality BC and the BC Restorative Circle, brought together social sector leadership, with an emphasis on health leadership, to develop and enhance systems understanding of a Restorative Approach. The focus of the symposium was at the governance, executive and management levels but included discussions of preventing and healing from harms in clinical practices and dispute resolution processes.
Gratitude
The BC Restorative Circle would like to extend their gratitude to Coast Salish Knowledge Sharer Carla George and Métis Elder Barb Hulme for sharing their wisdom and knowledge in opening and closing both days of the symposium. Your strength, compassion, and love reverberated across our hearts and minds and set the tone to role model restorative leadership.
Keynote Speakers and Panel Discussions
What is a Restorative Approach? Why & How it Matters for Health Care
Restorative Health Systems: Lessons from New Zealand
Shifting Paradigms to Identifying & Responding to Harm in Health Care
Panel Discussion: Understanding & Integrating a Restorative Approach
Panel Presentation: The Application of a Restorative Approach in BC
Panel Discussion #3: Considering Legal and Legislative Spaces
Patient Reflection: Bringing it All Together
Working Together to Adopt a Restorative Approach
The symposium attendees engaged in a live Thought Exchange, which is an online engagement platform in which they identified challenges and barriers, opportunities, and next steps that were discussed throughout two breakout sessions at the symposium. Key themes of the feedback highlight the multifaceted challenges and considerations involved in implementing a Restorative Approach, emphasizing the need for education, cultural humility, trust-building, and a shift in systemic attitudes and structures. The following is a consolidated summary of the feedback from the Thought Exchange, and from the Q&A sessions with panelists.
Challenges and Barriers
Opportunities
Next Steps for System Enhancement
Systemic coordination to guide the adoption of a Restorative Approach is provided by the BC Restorative Circle. Next Steps from the Restorative Leadership Symposium implicate leaders from multiple social sectors and emphasize the need to align efforts across legal, financial, and health systems.
- Maintain Momentum with Increased Inclusion and Collaboration
- Partner and engage with First Nations and Métis Nation BC to understand and advance Indigenous perspectives on adopting a Restorative Approach to ensure that it is a culturally safe and appropriate approach to responding to the unique nature of colonial processes, systems of white supremacy, and Indigenous-specific racism. Focus on relational and trauma-informed approaches.
- The BC Restorative Circle to host follow-up events to the Restorative Leadership Symposium.
- Support Capacity Development and The Prioritization of a Restorative Approach
- Support education, learning and development in collaboration with health system, education, and legal professionals, and patient partners. Develop learning resources including frameworks, principles, and ‘guardrails’ to guide the adoption of a Restorative Approach.
- Identify change leaders to role model cultural humility and restorative practices and champion a Restorative Approach.
- Prioritize a Restorative Approach with adequate resourcing for organizational change and capacity development at all levels.
- Support system learning through transparency, information sharing, and accountability throughout change leadership and change management processes.
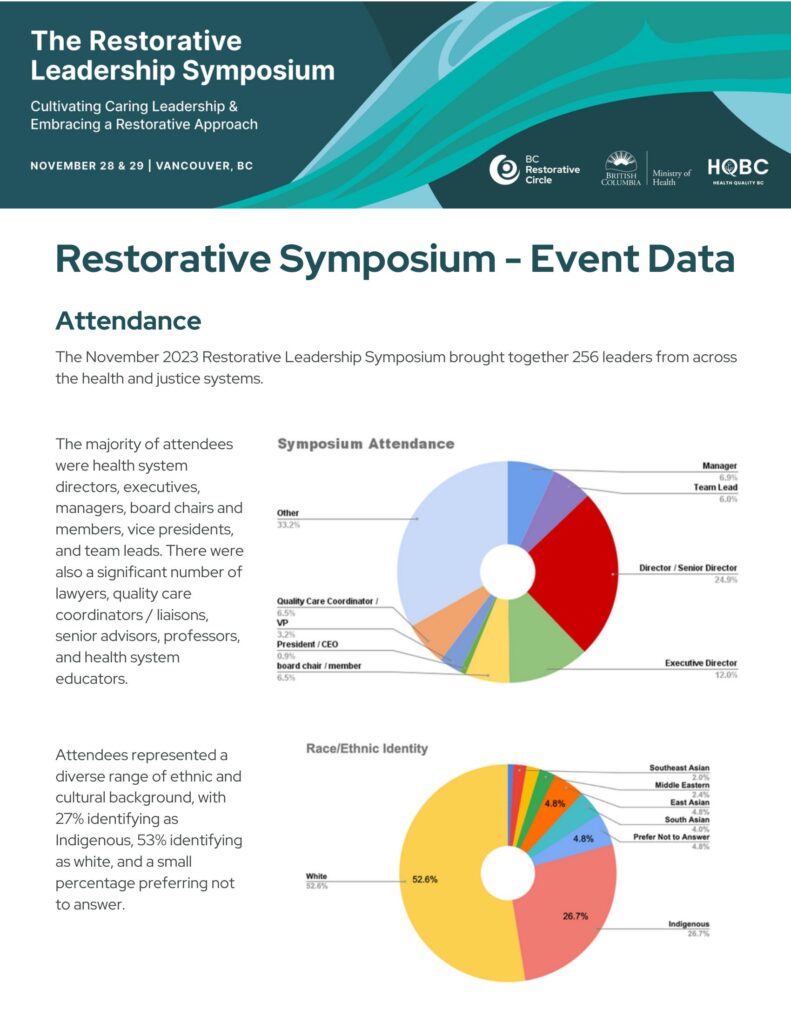
See the Data Gathered Post-Event
This report provides an overview of the data gathered from the Restorative Leadership Symposium.